COOPERATIVE EXTENSION
UNIVERSITY OF CALIFORNIA
ENVIRONMENTAL TOXICOLOGY NEWSLETTER
Vol. 16 No. 1, February 1996
In This Issue
Mercury Exposure in a Residential Community — Florida, 1994
Residential exposure to elemental mercury typically involves small amounts (e.g., the approximately 0.3 mL in a thermometer). During August 1994, five children residing in a neighborhood in Palm Beach County, Florida, found 5 pints of elemental mercury in an abandoned van. During the ensuing 25 days, the children shared and played with the mercury outdoors, inside homes, and at local schools. On August 25, 1994, a parent notified local police and fire authorities that her children had brought mercury into the home. On the same day, 50 homes were immediately vacated and an assessment of environmental and health impacts was initiated.
Door-to-door interviews of the entire neighborhood (n=363) were conducted, and a decontamination facility was established at the civic center. Based on information collected during the initial survey, residential structures and several classrooms at the local high school were tested for the presence of mercury. Ambient air samples (i.e., adult breathing zone grab samples collected approximately 5 feet above the floor) were collected in affected structures during the 6 days following the report of children handling mercury. In addition, during August 25-29, initial blood and urine samples were collected from potentially exposed persons and analyzed for mercury levels.
A total of 58 residential structures were monitored for indoor mercury vapor concentrations; unsafe indoor air levels of mercury (>15 mg/m;) were detected in 17, prompting the immediate evacuation of 86 persons. Several classrooms at the local high school were determined to be contaminated. This school was closed for 4 days until clearance air sampling indicated that the mercury level was <10 mg/m;. This level of mercury was considered safe for students and teachers rotating among the rooms for 50-minute classes. Pregnant women and young children were excluded from entering classrooms until mercury levels decreased to <0.3 mg/m;.
A total of 477 persons identified by the survey as potentially exposed were evaluated at the emergency department of the local hospital or the health department clinic for mercury poisoning by testing both blood and urine specimens for total inorganic mercury levels. Elevated blood and/or urine mercury levels were detected in 54 persons: blood levels ranged from 1.1 mg/dL to 5.5 mg/dL (normal: <1 mg/dL) and urine levels ranged from 21 mg/L to 66 mg/L (normal: <20 mg/L). Ambient air samples ranged from 6.5 mg/m; to 300 mg/m;. Although these 54 persons were asymptomatic, concentrations of mercury detected in their blood and urine were consistent with the levels of mercury detected in their homes.
Homes and classrooms were decontaminated by spreading powdered sulfur absorbent on the floors and vacuuming surfaces with high efficiency particulate-arresting (HEPA) filters. Contaminated items (e.g., carpeting, padding, linoleum, clothing, bedding, vacuum cleaners, furniture, and washing machines) were removed and taken to a hazardous waste facility, and some homes required ventilation for periods up to 3 months. Because of the potential for residential exposure of many children and childbearing-aged women, an air mercury concentration of <0.3 mg/m; was established as a threshold at which families would be permitted to return to their homes. Ambient air samples were collected 24 inches above the ground (i.e., a child’s breathing zone), under normal living conditions for at least 8 hours.
By December 1, 1994, all displaced families had been permitted to return to their homes, and urine mercury levels of all exposed persons decreased.
Editorial Note: Most poisonings associated with exposure to elemental mercury occur in occupational settings, and reports of nonoccupational elemental mercury vapor poisonings are rare, especially in community-based settings. The exposures described in this report primarily affected homes and schools.
Inorganic mercury is a heavy, silver-white metal that is liquid at room temperature. The vapor pressure of mercury is high compared with other metals, creating the continual hazard of airborne exposure to mercury vapor, which is odorless and colorless. Mercury is absorbed into the blood following inhalation and is then transported to the brain and other areas of the nervous system and to all other tissues.
The development of clinical manifestations as the result of inhalation of mercury vapor is related to several factors, including the concentration of vaporized mercury, length of exposure, and individual susceptibility. Acute exposure to elemental mercury produces symptoms of metallic taste, burning, irritation, salivation, vomiting, diarrhea, upper gastrointestinal tract edema, abdominal pain, and hemorrhage. Symptoms of high levels of exposure usually begin abruptly and include fever, chills, malaise, nausea, coughing, shortness of breath, chest pain and tightness; the clinical course may progress to pulmonary edema and death. In comparison, chronic inorganic mercury poisoning can result in intention tremor, (This tremor is different from Parkinsonian tremor, which disappears during movement. Intention tremor occurs when movement is initiated and is not a "resting" tremor; Editor.) memory loss, insomnia, depression, irritability, excessive shyness, emotional instability, delirium, and acrodynia and may result in a neurologic syndrome known as "mad hatter syndrome".
The risks associated with mercury exposure are especially increased for children because mercury vapor is dense and settles and because children may be active on the floor or playing in dirt. In addition, because of lipid solubility, mercury crosses the placenta and is excreted in breast milk and, therefore, is a potential health hazard for unborn children and breast-feeding infants.
Elemental mercury is still widely used in industry for the manufacture of thermometers, barometers, vacuum pumps, and electrical components and may be present in household products such as cleaning solutions and adhesives. Small amounts of mercury, such as from a broken thermometer, can be cleaned up by spraying the mercury gently with hair spray or dusting with an absorbent such as powdered sulfur and sweeping up the mercury and absorbent with a whisk broom. After cleaning the spill, the broom should be securely bagged and discarded. Any person who discovers a large quantity of mercury should immediately contact the local poison-control center or health department.
The residential exposure described in this report was unprecedented in terms of the amount of mercury involved and the extent of contamination. The rapid and coordinated response to this incident minimized the risk for and assured the health of the exposed residents.
REF: Morbidity and Mortality Weekly Report (MMWR), 44(23), June 16, 1995. ■
New Cancer Risk Assessment Guidelines
Previous decisions made by EPA against pesticides and other chemicals could be re-reviewed under the agency’s new, less conservative "Proposed and Interim Guidelines for Carcinogen Risk Assessment," EPA officials noted recently. The new guidelines do not use Q* (Q*, or Q-star, is a measure of carcinogenic potency).
The draft guidelines, which are being revised in response to comments from within EPA, are expected to be published for comment about September 25.
The core of the new guidelines is use of ED10 (defined as the effective dose corresponding to 10% extra risk, adjusting for background incidence) as a starting point for linear extrapolation. ED10 is the dose of a chemical that exerts an effect on 10% of a group being studied. It is the starting point for developing a dose-response model. The new guidelines have three, rather than the current six (A,B,C,D, etc.), descriptors for classifying human carcinogenic potential: "known/likely," "cannot be determined," and "not likely."
The agency plans to begin using the new guidelines after October 1, 1995.
The new guidelines, according to EPA, emphasize an agent’s mode of action "To reduce the uncertainty in describing the likelihood of harm and in determining the dose response approach(es). This emphasis should provide incentive for generating key information needed to reduce the default assumptions used in risk assessment."
There are three default approaches in the guidelines, EPA noted: "linear, nonlinear, or both. Curve fitting in the observed range would be used to determine the effective dose corresponding to 10% extra risk (ED10). The ED10 would then be used as a starting point for extrapolation to the origin as the linear default or for derivation of a margin of exposure (MOE) as the nonlinear default. In determining the adequacy of the MOE, biological information concerning such factors as human variation and species differences would be taken into consideration."
"Biological based extrapolation model is the preferred approach for quantifying risk. It is anticipated, however, that the necessary data for the parameters used in such models will not be available for most chemicals. The new guidelines allow for alternative quantitative methods, including several default approaches."
Three Descriptors for Classifying Carcinogen Potential - The three descriptors for human carcinogenic potential that will replace the old alphanumeric category system will be "known/ likely," "cannot be determined" and "not likely," the guidelines said. They are defined as follows:
"Known/Likely"
Appropriate when the weight of evidence provides reasonable assurance of carcinogenic potential for humans, this group of carcinogens includes:
• agents known to be carcinogenic in humans based on either epidemiologic evidence or a combination of epidemiological and experimental evidence, demonstrating causality between human exposure and cancer;
• agents with epidemiological data that show a plausible causal association and experimental evidence or a strong experimental basis that should be treated as if they were known human carcinogens, and
• agents that are likely to produce cancer in humans due to the production or anticipated production of tumors by modes of action that are relevant or assumed to be relevant to human carcinogenicity.
"Cannot Be Determined"
This group of descriptors is appropriate whenever support for a conclusion about carcinogenic potential for humans is not sufficient to proceed with the risk assessment, the guidelines said. Further testing is needed. Examples of these include:
• agents whose carcinogenic potential cannot be determined, but for which there is suggestive evidence that raises concern for carcinogenic effects;
• agents whose carcinogenic potential cannot be determined because the existing evidence is composed of conflicting data (there is evidence leading in two different directions);
• agents whose carcinogenic potential cannot be determined because there are inadequate data to perform an assessment, and
• agents whose carcinogenic potential cannot be determined because no data are available to perform an assessment.
"Not Likely"
This is the appropriate descriptor when evidence about an agent, either generally or about a condition of exposure, is satisfactory for deciding that there is no basis for human hazard concern, the guidelines said. Examples include:
• agents not likely to be carcinogenic to humans because they have been appropriately evaluated in animals without demonstrating carcinogenic effects;
• agents not likely to be carcinogenic to humans because they have been appropriately evaluated in animals without demonstrating carcinogenic effects that are relevant to humans (e.g., showing only effects in the male rat kidney due to accumulation of alpha2u-globulin), and
• agents not likely to be carcinogenic to humans below a dose range because they have been appropriately evaluated in animals and the only effects show a dose range limitation.
REF: Pesticide & Toxic Chemical News, 23(43-44) as noted in Kansas Pesticide Newsletter, 18(9), September 15, 1995. ■
Surface Dust on Hands Used to Assess Childhood Lead Exposure
"When it comes to environmental health and community health, the needs of our children should be paramount," said Lynn Goldman, assistant administrator for the EPA’s Office of Prevention, Pesticides and Toxic Substances. "The assessment of risk for children makes a difference, particularly with respect to lead poisoning."
For assessment of lead exposure in children, Howard Mielke, environmental toxicologist for the Xavier Institute of Bioenvironmental Toxicology, Xavier University of Louisiana, New Orleans, discussed one type of exposure assessment method that is more sensitive to the actual site where children play. In New Orleans, Mielke and his team used hand wipes to identify relevant sources of lead exposure at child-care centers, selected from innercity and suburban communities with known high and low lead levels in soil.
Soil containing above-average levels of lead (exceeding the rural background level of 25 micrograms [mg] (25 ppm) of lead per gram of soil) has been contaminated with man-made lead sources such as lead-based paint, leaded gasoline, or industrial or incinerator emissions. Lead dust from all of these sources accumulates in soil, which becomes an environmental carrier of lead to animals and humans. In 1993, Bourgoin et al estimated that the total tolerable daily intake (TTDI) of lead ingested from all sources is 6 mg (Am J of Public Health 83:1155-1160). For children under 6 years of age, ingestion above 6 mg of lead per day is associated with an increase in body burden for lead.
The study included 15 child-care centers and 145 children. Samples collected for the New Orleans child-care study included indoor and outdoor surface wipes, outdoor soil samples when present, and hand wipes of children before and after outdoor play. They could not determine specifically how much lead the children ingested through hand-to-mouth contact.
Overall, lead on children’s hands increased from 1.73 mg of lead per hand before outdoor play to 3.75 mg of lead per hand after outdoor play. Thus, the children exhibited higher lead levels on their hands after they were exposed to the outdoor environment than when they left the indoor environment. "The play areas of the child-care centers varied in quality," Mielke explained. "With play areas that had no soil, hand wipes revealed little if any increases in lead dust exposure after outdoor play. In those play areas that contained soil, the lead dust on hands generally increased after outdoor play, sometimes to levels above 10 mg per hand." Generally, children at private child-care centers had higher lead levels on their hands than children at public child-care centers.
Mielke added that the findings from this study have direct bearing on lead sources and risks to which children are exposed as part of their daily experience when they attend child-care centers in New Orleans. "Given a total tolerable daily intake of 6 mg of lead per day from all sources, some child-care centers presented conditions where children are at an excessive risk of lead exposure," he said. "Child-care centers were very responsive to the results, and within a few days, the suggested soil sites of the lead were cleaned up [by replacing the soil with brick blocks or bark chips]." Increased child supervision also ensured that the children would not play near areas that were problematic.
REF: Health & Environment Digest, 9(6), October 1995. ■
Child Safety and Pesticides
Although pesticides can be beneficial to society, they can be dangerous if used carelessly or if they are not stored properly and out of the reach of children. According to data collected from the American Association of Poison Control Centers, in 1993 alone, an estimated 80,000 children were involved in common household pesticide-related poisonings or exposures in the United States.
A survey by the US. Environmental Protection Agency regarding pesticides used in and around the home revealed some significant findings:
* Almost half (47%) of all households with children under the age of five had at least one pesticide stored in an unlocked cabinet, less than 4 feet off the ground (i.e., within the reach of children).
* Approximately 75% of households without children under the age of five also stored pesticides in an unlocked cabinet, less than 4 feet off the ground (i.e., within the reach of children). This number is especially significant because 13% of all pesticide poisoning incidents occur in homes other than the child’s home.
Bathrooms and kitchens were cited as the areas in the home most likely to have improperly stored pesticides. Examples of some common household pesticides found in bathrooms and kitchens include roach sprays; chlorine bleach; kitchen and bath disinfectants; rat poison; insect and wasp sprays, repellents and baits; and, flea and tick shampoos and dips for pets. Other household pesticides including swimming pool chemicals and weed killers. (From: Pesticide Coordinator Report, Washington D.C.)
REF: Kansas Pesticide Newsletter, 18(6), June 14, 1995. ■
Economic Costs of Birth Defects and Cerebral Palsy - United States, 1992
Birth defects are the leading cause of infant mortality in the United States and the fifth leading cause of years of potential life lost. Despite the substantial allocation of medical and nonmedical resources to the care and support of persons with birth defects, the economic costs of such defects have not been estimated accurately. Because estimates of the cost per new case of a birth defect represent the savings from preventing a case, an incidence-based approach enables assessment of the value of prevention strategies. This approach was used to estimate the cost of illness for cerebral palsy and for 17 of the most clinically important structural birth defects in the United States. This report uses data from California (adjusted to provide national estimates) and national data to estimate the costs of these 18 conditions occurring in the United States during 1992.
The number of new cases of the conditions were estimated using data from the California Birth Defects Monitoring Program (CBDMP). Estimates of age-specific direct costs of the conditions were based on reported charges and expenditures for children with the conditions.
For 1992, the combined estimated cost of the 18 conditions in the United States was $8 billion. Costs ranged from $75,000 to $503,000 per new case. Conditions with the highest costs per case were characterized by relatively high levels of long-term activity limitations (e.g., cerebral palsy [$503,000], Down syndrome [$451,000], and spina bifida* [$294,000]). In addition, these conditions had among the highest total lifetime costs ($2.4 billion, $1.8 billion, and $489 million, respectively), reflecting their relatively high incidences.
*Spina bifida is incomplete closure of the spinal cord during embryonic development.
REF: MMWR, 44(37), September 22, 1995. ■
Symptoms of Substance Dependence Associated with Use of Cigarettes, Alcohol, and Illicit Drugs — United States, 1991–1992
Each year in the United States, approximately 400,000 deaths result from cigarette smoking, 100,000 from misuse of alcohol, and 20,000 from use of illicit drugs. Many of the adverse health effects associated with the use of tobacco, alcohol, and illicit drugs result from long-term use caused by substance dependence (i.e., addiction) -- a cluster of cognitive, behavioral, and physiological symptoms indicating sustained psychoactive substance use despite substance-related problems. In addition, substance dependence is characterized by repeated self-administration that usually results in tolerance, withdrawal, and compulsive drug-taking behavior. Nicotine is the psychoactive substance in cigarettes and other forms of tobacco that accounts for the addictive properties of tobacco. In addition to tobacco, other potentially addictive substances include alcohol, marijuana, and cocaine. To assess the prevalence of selected indicators of substance dependence among the U.S. population, the Centers for Disease Control and the National Institute on Drug Abuse analyzed data from the National Household Survey on Drug Abuse (NHSDA) for 1991-1992. The findings in this report suggest that a symptom of substance dependence is more likely to be reported by persons who smoke cigarettes and persons who use cocaine than by persons who use alcohol or marijuana.
Information about the indicators of dependence was based on responses to four questions; persons who reported current use of cigarettes, alcohol, marijuana, or cocaine were asked whether, during the 12 months preceding the survey, they 1) "felt [they] needed or were dependent on [the substance]," 2) "needed larger amounts to get the same effect," 3) "felt unable to cut down on [their] use even though [they] tried," and 4) "had withdrawal symptoms, that is, felt sick because [they] stopped or cut down on [their] use." The analysis of "unable to cut down" and "felt sick" was restricted to persons who reported trying to reduce their substance use during the preceding 12 months.
Of the 61,426 total NHSDA participants during 1991-1992, use of cigarettes, alcohol, marijuana, or cocaine during the 30 days preceding the survey was reported by 14,688 (26.6%), 27,814 (49.4%), 3904 (4.6%), and 821 (0.8%) persons, respectively. Daily use of these substances for >2 consecutive weeks during the 12 months preceding the survey was reported by 78.4% of persons who smoked cigarettes, and by 22.6%, 13.8%, and 12.4% of those who used marijuana, alcohol, and cocaine, respectively. Cigarette smokers were more likely than persons who used the other substances to report having tried to cut down, and were approximately twice as likely as persons who used alcohol, marijuana, or cocaine to report having been unable to cut down. Cigarette smokers were more likely than users of the other substances to report feeling dependent on the substance or feeling sick when they stopped or cut down on its use. Cigarette smokers (75.2%) were more likely to report one of the four symptoms of dependence than were persons who used cocaine (29.1%), marijuana (22.6%), or alcohol (14.1%).
Editorial Note: The findings in this report suggest that persons who smoked cigarettes and persons who used cocaine were more likely than those who used alcohol or marijuana to report a symptom of substance dependence after controlling for frequency of use. The high level of dependency associated with cigarette smoking may account, in part, for the low success rate for attempts to quit smoking (only 2.5% of smokers successfully quit each year) even though most smokers report wanting to quit smoking. In addition, a high proportion (73%) of adolescents who smoke but who intended to quit smoking in 5-6 years were still smoking 5 years later.
REF: MMWR, 44(44), November 10, 1995. ■
Increasing Morbidity and Mortality Associated with Abuse of Methamphetamine — United States, 1991–1994
Methamphetamine (also known as "speed," "crystal," "crank," "go," and "ice") is the most widely illegally manufactured, distributed, and abused type of amphetamine, a class of stimulant drugs. An estimated 4 million persons in the United States have abused methamphetamine at least once. Information from several sources -- including medical examiners, hospital emergency departments (EDs), substance-abuse-treatment facilities, and community epidemiologists -- suggests a recent increase in morbidity and mortality associated with abuse of methamphetamine in the United States, primarily in the West but also in the South and Midwest.
From 1991 to 1994, the number of methamphetamine-related deaths reported by medical examiners nearly tripled from 151 to 433. The number of methamphetamine-related deaths increased by 850% in Phoenix, 238% in San Diego, 144% in San Francisco, and 113% in Los Angeles. In 1994, most of the 433 decedents were aged 26-44 years (284 [66%]), male (345 [80%]), and white (343 [80%]). Nearly all the deaths (398 [92%]) involved methamphetamine in combination with at least one other drug, most often alcohol (128 [30%]), heroin (98 [23%]), or cocaine (92 [21%]).
Editorial Note: Methamphetamine is often abused with other drugs (e.g., alcohol, cocaine, or heroin) and can be "snorted," injected, or smoked. One mode of administration may dominate in a particular area. Methamphetamine abusers have reported physical symptoms that include weight loss, tachycardia, tachypnea, hyperthermia, insomnia, and muscle tremors. The behavioral and psychiatric symptoms reported most often include violent behavior, repetitive activity, memory loss, paranoia, auditory hallucinations, and confusion or fright.
REF: MMWR, 44(47), December 1, 1995. ■
REMINDER!
Public Health Recommendations to Prevent Air-Bag-Associated Injuries to Infants and Children
• All infants and children should be properly restrained in child safety seats or lap and shoulder belts when riding in a motor vehicle.
• Infants riding in rear-facing child safety seats should never be placed in the front seat of a car or truck with a passenger-side air bag.
• Children should ride in a car’s rear seat. If a vehicle does not have a rear seat, children riding in the front seat should be positioned as far back as possible from an air bag.
REF: MMWR, 44(45), November 17, 1995. ■
National Drunk and Drugged Driving Prevention Month -- December 1995
Persons who drive while impaired by alcohol or other drugs are a public health hazard to themselves and to others. Although the injuries, disabilities, and deaths associated with impaired driving are preventable, in 1994, alcohol-related motor-vehicle crashes resulted in 16,600 deaths in the United States; approximately one third occurred among persons aged <25 years. Such crashes remain a leading cause of death for teenagers and young adults.
Approximately one third of deaths among persons aged 15-24 years result from motor-vehicle crashes. Although alcohol use increases the risk for motor-vehicle crashes for all drivers, for young drivers the risk begins to increase at very low blood alcohol concentrations (BACs). (See Figure 1 below)
Factors that may have contributed to the decline in both impaired driving and total alcohol-related traffic fatalities among young persons include prompt license suspension for persons who drive while intoxicated; increasing the minimum drinking age (since 1988, the minimum drinking age has been 21 years in all states); and the initiation of public education, community awareness, and media campaigns about the dangers of alcohol-involved driving.
REF: MMWR, 44(47), December 1, 1995. ■
TOX TIDBITS
Editorial Note
Shortly after Christmas last year while I was walking my dogs in the Sierra Foothills, I came upon some "trash" hidden behind some bushes on a logging road. A closer look revealed a 30 gallon, blue plastic drum, and several black plastic bags. The blue drum contained a small volume of liquid and some frothy residue which had a strong, organic solvent smell (like dry cleaning fluid). It was the remains of an illegal drug manufacturing laboratory, probably one which made methamphetamine. I contacted the local sheriff, and after investigating, the county hazardous waste removal team came and safely removed the waste. I was informed that such "trash" is quite often dumped in isolated areas.
Anyone who finds such suspicious "trash" should contact their local law enforcement agency for investigation. Do not take any chances with these wastes if you find them, they are indeed hazardous in terms of toxicity and flammability. Don’t sniff, and don’t try to remove them yourself! ■
E coli 0157:H7
Ground beef isn't the only source of Escherichia coli 0157:H7 infections, a source at the Centers for Disease Control and Prevention (CDC) told the National Meat Association (NMA). Less than half of the 1995 outbreaks reported to CDC through mid-September were caused by ground beef, NMA said. Other vehicles of infection included person-to-person, swimming, lettuce, water, and an "unknown" source. Two of the largest outbreaks resulted from person-to-person contact in day-care facilities.
REF: Food Chemical News, October 13, 1995. ■
Increasing Pneumococcal
Vaccination Rates Among Patients of a
National Health-Care Alliance -- United States, 1993
Streptococcus pneumoniae is the most common cause of bacterial pneumonia worldwide and a leading cause of sepsis and meningitis. In the United States, an estimated 40,000 persons die each year from pneumococcal infections. Since 1983, 23-valent pneumococcal polysaccharide vaccines have been licensed in the United States and are 56%-57% effective in preventing invasive pneumococcal disease. However, the 1993 National Health Interview Survey documented that <28% of persons in high-risk categories, including all persons aged >65 years, reported ever having received the vaccine.
REF: MMWR, 44(40), October 13, 1995. ■
Fatal Lab Acid Spill
On October 28, 1994, in a small Western Australia laboratory, a man died after he accidentally splashed about 100 ml of a 70% solution of hydrofluoric (HF) acid on his leg. The 37-year-old employee jumped into a nearby swimming pool in a futile attempt to neutralize the toxic chemical. In an effort to save his life, doctors amputated the lab worker's leg. Unfortunately, the acid had already poisoned the victim's blood system and he died the following day.
Hydrofluoric acid has to come in contact with only 2% of the body to be fatal. Therefore, the victim had little chance of surviving a hydrofluoric acid spill as extensive as this, even if immediate first aid had been administered. Hydrofluoric acid is commonly found in campus laboratories and may be used for a wide variety of applications at varying strengths. In Australia, a special permit must be obtained to use HF and a neutralizing agent, calcium gluconate gel, must be kept on site.
REF: Vet Human Toxicol, 37(6), December 1995. ■
Cutting Boards
An article in the summer 1995 Agriculture and Agri-Food Canada's Foodborne Disease Bulletin revisited the debate over whether wooden or plastic cutting boards are safer. The article went against the prevailing wisdom and found that wood was better than plastic, but that University of Michigan microbiologists later found through electron microscopy that bacteria were still viable on wooden cutting boards. The article quoted Dr. Mansell Griffiths, a University of Guelph microbiologist, as saying that as long as surfaces are maintained in a hygienic fashion and sanitized frequently, there should be no danger of cross-contamination from either a butcher's block or a plastic block. Griffiths further muddied the debate by saying the ideal cutting board for commercial operations would be stainless steel, but he added that it would be "prohibitively expensive and impractical."
REF: Food Chemical News, 37(34), October 16, 1995. ■
Centers for Disease Control
(CDC) Blames 1994 Botulism Outbreak on
Cooked Potatoes Held in Foil
A "reportedly baked" potato wrapped in aluminum foil and held at room temperature for 18 hours apparently was the source of botulism that sent 29 people to the hospital in El Paso, Texas, in April 1994. All the patients ate either skordalia (cold potato and garlic dip) or eggplant dip. Botulism toxin type A was detected in both skordalia and eggplant dip. Skordalia contained a potato that was reportedly baked, wrapped in aluminum foil and then held at room temperature in the foil for 18 hours. No other ingredient in the restaurant was unique to skordalia, and none of the other ingredients tested had botulism toxin. Skordalia apparently contaminated the eggplant dip in the adjacent container via shared utensils.
The foil provides the anaerobic environment necessary for toxin production. Food preparers and consumers should be alerted to the hazards of holding cooked potatoes wrapped in aluminum foil at ambient temperatures.
REF: Food Chemical News, 37(33), October 9, 1995. ■
Less Than 5-10% of Commercial Chemicals Viewed as Human Carcinogens
Toxicologists with the National Institutes of Health have concluded that less than 5-10% of the 75,000 chemicals in commercial use "might be reasonably expected to be carcinogenic to humans."
The NIH scientists reported that slightly more than half of the 400 chemicals tested (52%) induced cancer in at least one organ of one sex of one species of the four sex/species groups typically used by the National Cancer Institute/National Toxicology Program (NCI/NTP). Only 92 of the test chemicals (23%) were positive in two species and thus by international criteria considered likely to pose a carcinogenic hazard to humans.
"The majority (80%) of the 133 chemicals selected only on production/exposure considerations were not carcinogenic in animals, even when tested at the maximum tolerated (or minimally toxic) dose. Only nine (6.8%) were positive in two species, and none is listed in the International Agency for Research on Cancer (IARC) groups 1 or 2A," the NIH scientists reported, concluding:
"Therefore, we predict that if all 75,000 chemicals in use were to be tested for carcinogenicity in the standard NTP bioassay, significantly less than 50% would be carcinogenic in animals, and an even smaller percentage (less than 5-10%) would need further evaluation."
The authors nonetheless endorsed IARC's view that, in the absence of adequate human data, "it is biologically plausible and prudent to regard agents and mixtures for which there is sufficient evidence of carcinogenicity in experimental animals as if they presented a carcinogenic risk to humans."
REF: Food Chemical News, 37(26), August 21, 1995. ■
Diabetes, Heart Disease from Agent Orange?
A Defense Department study of Air Force veterans exposed to Agent Orange during the Vietnam War found no increase in cancer risk but did find possible links to diabetes and heart disease.
REF: Washington Times, October 7, 1995. {EPA Newsbreak} ■
Lawyers Stress Fiscal Benefits of Smoking
According to tobacco industry lawyers, cigarette smoking has beneficial effects: tax revenues from the sale of cigarettes; revenues from doctors and health-care providers who treat smoking-related illnesses; and the premature deaths of smokers saves the state money since they spare taxpayers the cost of long-term geriatric care.
REF: Wall Street Journal, September 6, 1995. {EPA Newsbreak} ■
DuPont Labels, MSDSs on Internet
Specimen labels and material data safety sheets for DuPont products are available from the Internet. The information may be accessed from the Internet via the World Wide Web (WWW) at the following address: http://aginfo.trinet.com/.
REF: Agrichemical and Environmental News, 116, October 1995. ■
![]() VET NOTES
VET NOTES ![]()
Fumonisin Dubbed 'Mycotoxin of The '90s' by Schwetz
Although fumonisins are the "mycotoxins of the ’90s," Bernard Schwetz of the National Center for Toxicological Research explained that more than 50 countries including the United States currently regulate aflatoxin and about a dozen other mycotoxins are regulated by one or more of 30 other countries. "There isn’t one voice as to what are the most important mycotoxins," he noted.
Mycotoxin research, although plentiful, has been plagued by the fact that the substances being tested are often mixtures and by-products of toxins, not a single, purified strain. "There are a lot of toxic effects (associated with mycotoxins), but it’s difficult to tell exactly which mycotoxin is causing the effect," Schwetz explained.
Fumonisins are "unique toxins," said William Norred of USDA's Russell Research Center in Athens, Ga. Aside from causing a wide variety of toxic effects in different animals, they are water soluble, carcinogenic promoters (but probably not initiators), and act by causing the buildup of free sphingoloid bases in the cell, he said.
Perhaps the most important consideration for humans is that fumonisins are associated with esophageal cancer in two regions - one in South Africa and another in China - that have high corn consumption levels, Norred said. In both areas the population is poor, tends to eat corn as its staple food, and will consume products made from moldy corn (often used in the production of alcoholic beverages).
Norred added that he is currently trying to determine why one area in China that has a much lower level of esophageal cancer seems similar in other respects to the high-cancer area.
One potential problem with regulating fumonisins is that their major fungal producer, Fusarium moniliforme, exists inside seeds and can be transmitted through seeds to seedlings, making most traditional fungicides - which remove fungus from the outsides of seeds and plants - useless.
Charles Bacon of the Russell Research Center said he had conducted a study in which a kernel of corn was soaked in full-strength household bleach for 2.5 minutes - and the fungus still developed from the kernel.
Another problem with regulating fumonisin is that the fungus can exist inside plants in the spaces between plant cells, without leading to disease in the plants. Between 50% and 75% of corn plants "have symptomless expression" Bacon said.
Because of the prevalence of symptomless expression, "good-looking kernels can be just as toxic as moldy-looking kernels" of corn, Bacon said, although on average "good" corn has lesser levels of fumonisins than moldy corn.
Fumonisin Mode of Action Linked to Sphinganine Blockage
Fumonisins’ toxic effects are linked to sphingolipids in cells. The toxin blocks two important pathways in the normal life process of a cell, causing dramatic increases in the amount of a biologically active substance called sphinganine.
One matter of concern about the mode of action is that sphinganine levels stay elevated as long as fumonisin is present and afterwards.
Studies indicate that the sphingolipid effect does not seem to cross the placenta and affect rat fetuses, nor do high sphinganine levels in mother rats seem to affect the development of offspring.
The good news for people is that very little fumonisin accumulates in edible tissues of food animals, nor is there evidence that it accumulates in milk. Fumonisin risks for humans seem to come mainly through corn and corn products; the toxin has been shown to survive processing, although processing often significantly reduces the amount of toxin.
REF: Food Chemical News, 37(32), October 2, 1995. ■
Lasalocid (BovatecÔ) Induced Paralysis in Dogs
Most dogs (except beagles) are quite susceptible to lasalocid with a minimum toxic dose of approximately 10 to 15 mg/kg, while a dose in the 20 to 30 mg/kg is often lethal. Poisoning is characterized by acute progressive flaccid paralysis of skeletal muscles (appears very similar to botulism) and associated clinical signs. Five clinical cases of lasalocid poisoning in dogs have been observed over a two-year period. Cattle premix pellets containing the ionophore lasalocid (BovatecÔ) were the sources of exposure in all cases. Clinical signs of muscle weakness, depression, and inability to stand were observed within a few hours of consumption. The severity of signs and prognosis are dose dependent. Transient elevated CPK was measured in two dogs. Three mildly affected dogs showed good response in 24 hours with supportive care and nearly complete recovery in a few days. In the two most severely affected dogs, death followed marked muscle weakness and paralysis and respiratory arrest within a few hours of ingestion. Skeletal muscle tissue was available for examination from only one affected dog, but no lesions were observed. Early use of emetics and activated charcoal are recommended in cases of known exposure. Clients with farm dogs should be alerted to the hazard of lasalocid concentrates.
REF: Penn State Veterinary News, November 1995. ■
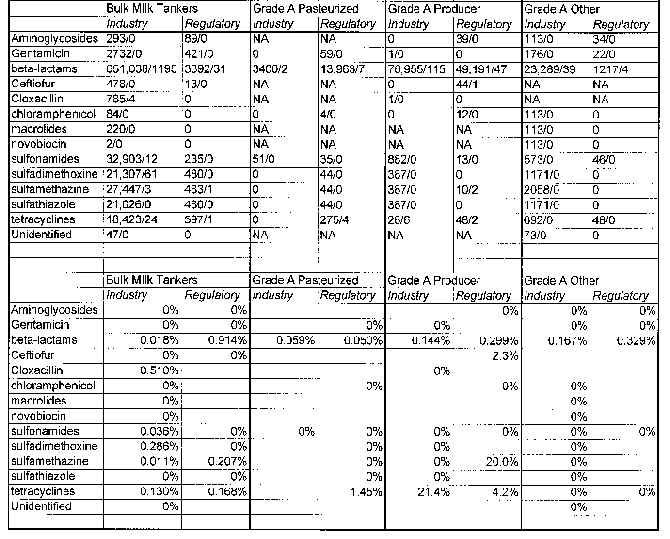
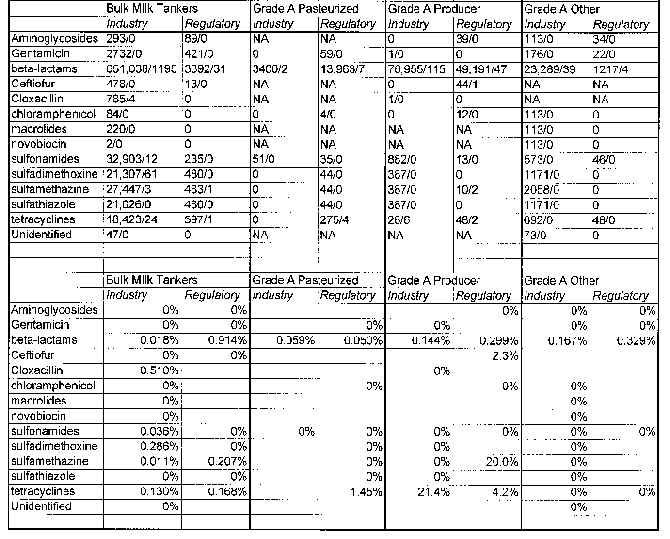
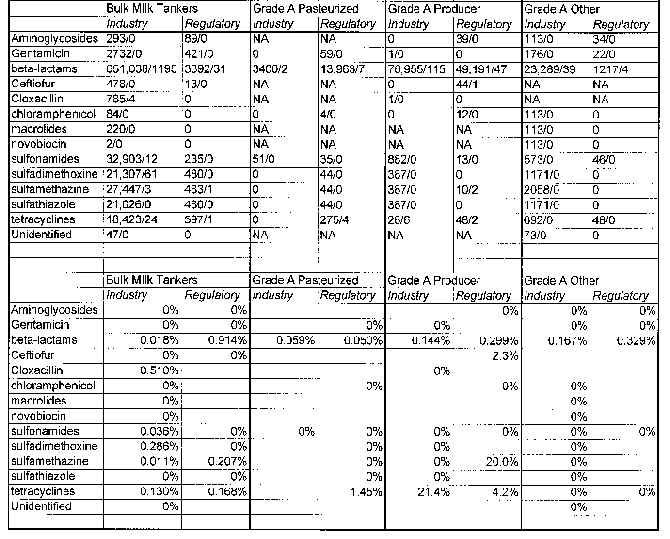
Milk Drug Residue 1st Quarter Report Shows 936 Positives Out of 934,513 Samples
Based on data received from 45 states, representing approximately 82% of the U.S. milk supply, the National Milk Drug Residue Data Base (NMDRDB) results for the first quarter of 1995 (Jan. 1-March 31) showed 936 positive samples out of 934,513 analyzed for animal drug residues.
The NMDRDB report, one of a series conducted by GLH, Inc., Falls Church, Va., under contract to the Food and Drug Administration, also noted that 1,077,168 tests were reported on the samples for 13 different groups of families or individual drugs. Thirty-nine separate testing methods were used to analyze the samples for residues, the report noted. The data are not intended for regulatory follow-up, FDA’s Milk Safety Branch said.
A sample is defined as "representing a load or lot of milk sampled and analyzed, e.g., a bulk milk pickup tanker, producer or over-the-road tanker, a silo, etc.," the report said, adding that data are reported by four sources of samples: bulk milk pickup tanker (bulk raw milk from a dairy farm); pasteurized fluid milk and milk products (after pasteurization, finished product in package form or bulk; includes milk, cream, condensed milk and dry milk products, and condensed and dry whey products); producer sample (raw milk obtained from a dairy farm; samples are reported by the permitting state, rather than by the analyzing state) and other (milk from silos, over-the-road tankers, etc.).
The report defined a "positive result" as meaning that a sample "was found to be positive for a drug residue by a test acceptable for taking regulatory action in a certified laboratory by a certified analyst or the milk was rejected on the basis of an initial test by the milk processors."
Broken out into sources, 759,985 samples were taken from bulk milk pickup tankers, of which 811 samples were positive (0.107%); 17,335 samples were taken from pasteurized fluid milk and milk products, of which 5 samples were positive (0.029%); 131,687 were producer samples, of which 113 were positive (0.086%); and 25,506 "other" samples were taken, of which 7 samples were positive (0.027%), the report said, adding that an objective of the NMDRDB "is to record every test run on each sample analyzed."
Since some samples are analyzed for more than one drug residue, the number of tests run is greater than the number of samples, the report noted, adding that, to avoid duplicate reporting of samples, the number of samples analyzed is reported separately from the number of tests run in the data base. Of the four sources of samples, the number of tests and positive tests were: bulk milk pickup tankers (893,689 total tests, 1,493 positive (0.167%)); pasteurized fluid milk and milk products (18,106 tests, 13 positive (0.072%)); producer samples (133,794 tests, 193 positive (0.144%)); and "other" samples (31,579 tests, 43 positive (0.136%)).
The table at the end of this newsletter lists the test results by family of drug and by individual drug.
REF: Food Chemical News, 37(36), October 30, 1995. ■
VET TOX TIDBITS
Center for Veterinary Medicine
The Center for Veterinary Medicine has established a home page on the World Wide Web. The home page may be found at http://www.cvm.fda.gov/ and includes Freedom of Information summaries on many new animal drugs, the FDA Approved Drug Products Database, some CVM guidelines, answers to frequently asked questions, information on CVM research activities and research plans, and the text of "FDA and the Veterinarian."
REF: Food Chemical News, 37(35), October 23, 1995. ■
Illegal Drugs
The Ohio General Assembly passed a bill in June making it a felony to administer illegal or unapproved drugs to livestock during exhibition. The law is a response to widespread use of illegal drugs on -- and other illegal means of tampering with -- show animals, particularly at youth livestock shows.
REF: Food Chemical News, 37(36), October 30, 1995. ■
Cat and Dog Bites
An estimated 1-2 million Americans are bitten by cats and dogs each year. Most victims are children who are bitten by dogs. Cat bite wounds on the hand have the greatest risk of infection. Pasteurella multocida, isolated in over half of all cat bite wounds and in 20-30 percent of dog bite wounds, can cause serious infection with severe complications.
Because most bites are not reported and do not require medical attention, a more accurate estimate (of the number of bites each year) cannot be provided. In the United States, persons with cat and dog bites account for 1 percent of all emergency department visits and over 10,000 hospitalizations annually. Ten to 20 dog-bite-related fatalities occur each year in this country; 70 percent of these victims are children under 10 years of age.
Large dogs can exert a pressure greater than 450 psi, which is enough to penetrate light sheet metal. Approximately 30-40 percent of cat bite wounds become infected; the incidence of infection in persons with dog bite wounds is 15-20 percent.
A mean of 2.8 to 3.6 bacterial species per wound are found in dog and cat bite wounds. When cultured, more than 80 percent of dog bite wounds yield potential pathogens, yet only 15-20 percent of these wounds become clinically infected. Predicting which wounds constitute the 15-20 percent that will become clinically infected continues to be a subject of considerable study.
REF: Florida Veterinary Scene, 4(10), Nov/Dec 1995. ■
Zoos Take Action on Antifreeze
The American Zoo and Aquarium Association has announced a national campaign to educate the public of the danger to animals from antifreeze. Animals die from drinking the liquid from puddles on the ground after it has leaked from vehicles or dumped illegally. Conventional antifreeze contains ethylene glycol, a poison that attacks the kidneys. The association is asking its 168 member zoos to convert their vehicles to a coolant that is made with propylene glycol.
REF: New York Times, October 8, 1995. {EPA Newsbreak} ■
National Milk Drug Residue Data
(Please note that the numbers are listed as # samples tested/# violative)
Art Craigmill
Extension Toxicologist
UC Davis