COOPERATIVE EXTENSION
UNIVERSITY OF CALIFORNIA
ENVIRONMENTAL TOXICOLOGY NEWSLETTER
Vol. 5 No. 4 September 1995
In This Issue
- Study Links Milk Overfortification, Hypervitaminosis D
- Toxicologist Sees Merit in Single Exposure Carcinogenesis
- Eye Injuries to Agricultural Workers -- Minnesota, 1992-1993
- Deaths from Melanoma -- United States, 1973-1992
- Reptile Associated Salmonellosis -- Selected States, 1994-1995
- Anticholinergic Poisoning Associated With an Herbal Tea -- New York City, 1994
- Self-Treatment With Herbal and Other Plant-Derived Remedies -- Rural Mississippi, 1993
- Etiology, Incubation Period and Clinical Syndrome for Common Foodborne Diseases
- TIDBITS
- Foodborne Botulism -- Oklahoma, 1994
- May the Imbiber Beware
- Methyl Bromide -- A Definite Maybe
- National Pesticide Telecommunications Network
- Inerts May be Cause of Certain Irritations
- PCBs in Fish and Fetal Toxicity
- Lyme Disease -- United States, 1994
- FDA Prohibits Use of Lead Solder in Cans Manufactured for Food
- Dietary Aluminum Poses No Significant Public Health Risk
- Ethics of Show Animal Drug Use Subject of Two Videos
- ettuce was Source of Montana E. coli Outbreak
- DA's BST Labeling Decision Upheld in U.S. District Court
- VET NOTES
- Half of all Feedlot Cattle Given Antibiotics Routinely
- Horse Outbreaks May Signify 'Bad' Fumonisin Year Ahead
- European Testing for Clenbuterol Residues Using Eye Tissues, Fluid
- Milk Drug Residues for FY 94 Reported
- CVM Will Look Closely at Sarafloxacin Use
- FDA Position on Extra-Label Use of Ionophore Drugs
- Neurotoxic Mycotoxins: A Review of Fungal Toxins that Cause Neurological Disease in Large Animals
Introduction
Once again the Environmental Toxicology Newsletter contains a potpourri of information on topics ranging from theories of carcinogenesis after single exposures, to Salmonellosis associated with handling pet reptiles. As we completed this issue, we received the latest information from the California Department of Pesticide Regulation about residues in produce in 1993 (the latest data). The next issue of this newsletter will contain these data and some figures that may be useful in presenting the information to the public. Stay tuned; we will get out at least 6 issues this year!
NEWS FLASH
A recent Compliance Policy Guide from the FDA Center for Veterinary Medicine excludes fluoroquinolones (e.g. enrofloxacin, sarafloxacin) from extra-label use in food animals. DO NOT USE FLUOROQUINOLONES IN FOOD ANIMALS. We will have more information in the next newsletter.
STUDY LINKS MILK OVERFORTIFICATION, HYPERVITAMINOSIS D
Following a recent outbreak of hypervitaminosis D in Massachusetts, researchers underscored the need for continued monitoring and enforcement of the vitamin D fortification process for dairy milk to prevent the disease that resulted in two deaths, said an article in the May 10 American Journal of Public Health.
Researchers from the Centers for Disease Control and Prevention and Massachusetts Department of Public Health confirmed that the outbreak of hypervitaminosis D in Boston resulted from the accidental overfortification in milk from a home-delivery dairy. Dairy inspections revealed that the instrument used to measure vitamin concentrate was broken, the study found. The Massachusetts outbreak prompted the Food and Drug Administration to initiate an ongoing survey of vitamin A and D levels in milk. In the first two years of the survey, fewer than one-third of the samples met the label claims for the vitamin.
"Hypervitaminosis D caused by overfortification of food is unusual; we could identify only one other occurrence," said the authors of the study, "An Outbreak of Hypervitaminosis D Associated with the Overfortification of Milk from a Home-Delivery Dairy."
"Nevertheless, the consequences of this episode highlight the importance of enforcing limits of vitamin D addition to milk," they found. While Massachusetts requires that fortification limits not exceed 500 IU per quart and that levels be checked biennially, milk samples from the implicated dairy exceeded state limits by 70 to 600 times, said the journal article.
Researchers also found a dose-response relationship between hyper-vitaminosis D and the number of years a person had consumed the dairy’s milk. Persons drinking the milk for five years or longer were at the highest risk, the study found.
Only 19 dairy consumers developed hypervitaminosis D, said researchers, who suggested that these consumers may have had a preexisting susceptibility for the disease. The dairy delivered milk to some 11,000 households.
Adjustments for vitamin D supplementation, cancer history, sunburn susceptibility and age did not alter the strong association between hyper-vitaminosis D and drinking the superfortified milk, they found.
Older age was a risk factor, they found, with 62% of case patients older than 60 years, compared with only 17% of the general population.
One reason may be the inability in this sensitive population to eliminate excess calcium due to decrease in renal function, researchers suggested.
The outbreak occurred between January 1985 and June 1991. While the disease is most frequently linked to patients taking vitamin D supplements, the study’s authors recommended that milk producers be educated about the risks of vitamin toxicity.
REF: Food Chemical News, 37(12), May 15, 1995. ■
TOXICOLOGIST SEES MERIT IN SINGLE EXPOSURE CARCINOGENESIS
An exhaustive search of the scientific literature on animal studies suggests that there may be considerable merit to the notion that a single exposure to some chemicals can cause cancer.
Dr. Edward Calabrese, professor of toxicology at the School of Public Health, University of Massachusetts, said the role of episodic exposures in carcinogenesis may be more important than previously recognized. He suggested that risk assessment procedures for less than lifetime exposures may need to be reassessed.
5,000 Positive Studies Found
He has found a total of about 5,000 positive studies involving 40 classes of chemicals and 400 individual chemicals.
Among the chemical classes involved, Calabrese said, are nitrosamines, nitrosoureas, aromatic amines, mycotoxins, polybrominated biphenyls, mustards, synthetic hormones including DES, triazenes, quinolines, sulfates, aldehydes and alcohol.
Calabrese defined single exposure to mean either a single gavage, a single dose by any route, inhalation for 24 hours or less, a single dermal application or, in the case of fish, exposure in water for 24 hours or less.
Calabrese said he looked at a variety of factors to see if there were things that might be tainting the results of his investigation. When he considered the possibility that the animals used in the study were limited, he found that the positive results appeared in 36 different mouse strains and 24 different rat strains. Similarly, the results were not limited to just a few journals. The positive results appeared in a wide variety of respected journals, with the most reports, 24 each, appearing in the Journal of the National Cancer Institute and Cancer Research, he noted. He said the positive results passed the scrutiny of "many different review panels ... over several generations of scientists."
"All of the evidence that I’ve seen suggests that these are genotoxic agents," Calabrese said.
Concern Over Raising Unnecessary Fears Expressed
Calabrese indicated that he has not published the results of his work in this area because of concerns about media treatment of the information and the fact that he is not certain that the suggestion of the possibility of developing cancer from a single exposure to a chemical necessarily has any relation to the risk of exposure.
In discussion following the talk, one audience member echoed this concern, saying, "This kind of list has the potential for scaring the hell out of people." He too noted the potential for "the misuse of this kind of list. ... You have to know what the dose is and what that means."
Calabrese said he has been working on putting his information into a database, the Single Exposure Carcinogen Database, that can be accessed by other scientists. He said it is time for other scientists to look at the information and begin to work with it so it is more widely tested and discussed.
REF: Food Chemical News, 37(10), May 1, 1995. ■
Eye Injuries to Agricultural Workers -- Minnesota, 1992-1993
During 1993, U.S. farm workers incurred an estimated 13,500 eye injuries that resulted in lost work time; many of these injuries could have been prevented.
Overall, 1359 farm household members living on 372 (68.5%) of 543 eligible farms were included in the survey; respondents were farm operators and selected adult household members. Farm injuries were defined as self-reported events related to farm operation that resulted in restricted activities for at least four hours, loss of consciousness, or seeking of medical care.
Respondents reported 106 farm injuries during the two periods (annual rate: 78.0 injuries per 1000 farm household members). Ten persons sustained 11 farm-related eye injuries (10% of all injuries and 8.1 eye injuries per 1000 farm household members).
Of the 11 farm-related eye injuries, four were caused by chemicals and seven by foreign bodies. Chemical-related eye injuries involved splashes of liquid agricultural chemicals (two cases) and fungicidal dust (one case); the fourth incident involved discovery of an eye injury in a child who had exited a chemical storage shed, although the details of the injury could not be ascertained. Foreign body-related injuries were sustained in association with activities including working with hand and power tools, welding, grinding, cutting metal, and augering grain. The injured person was reported to have been using eye protection in only one of these incidents. Medical care was sought for nine (82%) of the 11 injuries; seven required immediate medical attention. However, no residual problems or restrictions were reported by respondents; three of the 10 injuries to adults resulted in lost work time.
Farm operators also were asked about their use of protective equipment and/or procedures while performing specific work tasks involving potential dermal exposures to agricultural chemicals. For mixing or loading agricultural chemicals or for sprayer maintenance, 50% reported never wearing eye protection (e.g., goggles or safety glasses), and 9% reported never using protective gloves.
Of the 207 respondents who worked with anhydrous ammonia (an extremely caustic alkali that is stored under pressure and applied as a liquid fertilizer), 73 (35%) reported that they never or sometimes wore goggles, and 92 (44%) reported that they never or sometimes checked the water supply in their field emergency water tank.
Editorial Note: The Minnesota findings document the occurrence of eye injuries in a specific production-agriculture worker group -- farmers and household members living on family-operated farms -- and are consistent with other recent reports. For example, the Regional Rural Injury Study, a population-based survey in five midwestern states, documented an annual rate of 58.3 farm injury events per 1000 household members -- farm-related eye injuries accounted for 8.2% of all farm injuries. Based on the Traumatic Injury Surveillance of Farmers survey during 1993, the estimated 13,500 eye injuries among farm workers in the United States that resulted in lost time from work accounted for approxi-mately 6.7% of all lost-time injuries estimated for farming operations.
Based on the incident descriptions obtained, each of the 10 eye injuries to adults would most likely have been prevented if appropriate and well-fitting eye protection had been worn while those persons engaged in work with agricultural chemicals, power and hand tools, and grain- or seed-moving equipment. Personal protective equipment traditionally has not been considered a primary strategy for hazard control. The preferred strategies have included hazard substitution (i.e., replacing a hazardous chemical with a less hazardous one) and hazard isolation or use of engineering controls. Although these strategies are applicable in agricultural settings (e.g., use of closed pesticide-handling systems), use of eye protection provides a practical and cost-effective method of preventing eye injuries among farm workers. Goggles are recommended for chemical splash protection, and safety glasses with side shields can provide adequate protection (except in dusty environments) against flying particles or objects.
REF: Morbidity and Mortality Weekly Report (MMWR), 44(18), May 12,1995. ■
Deaths from Melanoma -- United States, 1973-1992
Approximately three fourths of all skin cancer-associated deaths are caused by melanoma. During 1973-1991, the incidence of melanoma increased approximately 4% each year. In addition, the incidence of melanoma is increasing faster than that of any other cancer. To characterize the distribution of deaths from melanoma in the United States, the Centers for Disease Control analyzed national mortality data for 1973 through 1992.
From 1973 through 1992, the overall percentage increase in the rate of deaths from melanoma (34.1%) was the third highest of all cancers; for males, the percentage increase for melanoma (47.9%) was the highest for all cancers. During the same period, the increase in the rate of deaths from melanoma was greater for white males than for other racial and sex groups. In 1992, the rate of deaths from melanoma was 5.9 times higher for whites than for all other races (2.5 and 0.4 per 100,000 population, respectively), and 2.1 times higher for males than females (3.1 and 1.5, respectively).
In every state, the rate of deaths from melanoma was substantially higher for whites than for persons of all other races.
During 1973-1975 and 1990-1992, death rates were highest for white men aged >50 years. The death rate increased more with age for males than for females during 1990-1992.
Editorial Note: The findings in this report indicate that the rate of deaths from melanoma was higher for whites than persons of all other races -- a finding consistent with the more common occurrence of melanoma among persons with lightly pigmented skin and an incidence among whites that is more than 10 times higher than that for blacks. Based on estimates by the American Cancer Society, during 1995 an estimated 34,100 new cases of melanoma will be diagnosed and 7200 deaths will be caused by melanoma. The likelihood of survival of melanoma is substantially greater if the disease is detected early and treated. Early detection of thin lesions is associated with improved prognosis and treatment outcome than is detection of thicker, later stage tumors.
Risk factors for melanoma related to ultraviolet radiation exposure include a history of sunburn or sun sensitivity, a tendency to freckle, the presence of lightly pigmented skin, blue eyes, and blond or red hair. Other risk factors include a family or personal history of melanoma and the presence of a large number of moles or any atypical moles. Sources for exposure to ultraviolet radiation include sunlight and artificial light (e.g., tanning booths), both of which can cause acute sunburn. The increased risk among persons who sustain intermittent, acute sunburn at an early age (i.e., <18 years) underscores the need for initiating prevention measures early in childhood.
Adults, particularly older men in whom rates of deaths from melanoma are highest, should be encouraged to perform periodic skin self-examination or be examined by a family member to monitor location, size, and color of a pigmented lesion or mole. The "ABCD approach" can be used to assess pigmented lesions and represents mole asymmetry ("A"), border irregularity ("B"), nonuniform color (i.e., pigmentation) ("C"), and diameter >6 mm ("D").
Recommendations for preventing melanoma should emphasize reduction of direct exposure to the sun when sunburn is most likely to occur, especially from 10 a.m. to 3 p.m. Specific measures include wearing a broad-brimmed hat and clothes that protect sun-exposed areas, seeking shade when outdoors, using a sunscreen of sun protection factor >15 that provides protection against ultraviolet radiation A and ultraviolet radiation B, and referring to the daily Ultraviolet Index rating provided by the National Weather Service and others when planning outdoor activities.
REF: MMWR, 44(17), May 5, 1995. ■
Reptile-Associated Salmonellosis -- Selected States, 1994-1995
During 1994-1995, health departments in 13 states reported to the Centers for Disease Control, persons infected with unusual Salmonella serotypes in which the patients had direct or indirect contact with reptiles (i.e., lizards, snakes, or turtles). In many of those cases, the same serotype of Salmonella was isolated from patients and from reptiles with which they had had contact or a common contact. For some cases, infection resulted in invasive illness, such as sepsis and meningitis.
Ohio. During January 1994, a 6-week-old boy was hospitalized because of diarrhea, stiff neck, and fever; culture of samples of blood and cerebrospinal fluid yielded Salmonella serotype Stanley. The infant was treated with intravenous cefotaxime for Salmonella sepsis and meningitis and discharged from the hospital after 56 days. He had been fed only formula and had not attended a child-care facility; household contacts were asymptomatic. The family had purchased a 4-inch water turtle in April 1993. A culture of stool from the turtle yielded Salmonella Stanley. Although the infant had not had contact with the turtle, other family members had had direct contact, and the turtle’s food and water bowls were washed in the kitchen sink.
Additional investigations. In addition to Ohio, 12 other states (Connecticut, New Jersey, New York, North Carolina, Pennsylvania, California, Colorado, Florida, Illinois, Minnesota, Oregon, and Utah) have reported recent isolation of the same Salmonella serotype from samples obtained from patients and reptiles with which they had been in contact or associated. Several of these states issued press releases about the risk for acquiring salmonellosis from reptiles. In addition, some states have issued health alerts to pet stores to warn owners and prospective owners about the risks for salmonellosis associated with contact with reptiles and to provide instructions about proper handling of reptiles; store owners have been asked to post the alert and provide copies to all persons purchasing a reptile.
Editorial Note: Reptiles are popular as pets in the United States: an estimated 7.3 million pet reptiles are owned by approximately 3% of households. Because the most popular reptile species will not breed if closely confined, most reptiles are captured in the wild and imported. The number of reptiles imported into the United States has increased dramatically since 1986 and primarily reflects importation of iguanas (27,806 in 1986 to 798,405 in 1993).
A high proportion of reptiles are asymptomatic carriers of Salmonella. Fecal carriage rates can be more than 90%; attempts to eliminate Salmonella carriage in reptiles with antibiotics have been unsuccessful and have led to increased antibiotic resistance. A wide variety of Salmonella serotypes has been isolated from reptiles, including many that rarely are isolated from other animals (reptile-associated serotypes). Reptiles can become infected through transovarial transmission or direct contact with other infected reptiles or contaminated reptile feces. High rates of fecal carriage of Salmonella can be related to the eating of feces by hatchlings -- a typical behavior for iguanas and other lizards -- which can establish normal intestinal flora for hindgut fermentation.
During the early 1970s, small pet turtles were an important source of Salmonella infection in the United States; an estimated 4% of families owned turtles, and 14% of salmonellosis cases were attributed to exposure to turtles. In 1975, the Food and Drug Administration prohibited the distribution and sale of turtles with a carapace <4 inches; many states prohibited the sale of such turtles. These measures resulted in the prevention of an estimated 100,000 cases of salmonellosis annually. However, since 1986, the popularity of iguanas and other reptiles that can transmit infection to humans has been paralleled by an increased incidence of Salmonella infections caused by reptile-associated serotypes.
Because young children are at increased risk for reptile-associated salmonellosis and severe complications (e.g., septicemia and meningitis), reducing exposure of infants or children aged <5 years to reptiles is particularly important. The risks for transmission of Salmonella from reptiles to humans can be reduced by avoiding direct and indirect contact with reptiles (see below).
Recommendations for Preventing Transmission of Salmonella
From Reptiles to Humans
• Persons at increased risk for infection or serious complications of salmonellosis (e.g., pregnant women, children aged <5 years, and immunocompromised persons such as persons with AIDS) should avoid contact with reptiles.
• Reptiles should not be kept in child-care centers and may not be appropriate pets in households in which persons at increased risk for infection reside.
• Veterinarians and pet store owners should provide information to potential purchasers and owners of reptiles about the increased risk of acquiring salmonellosis from reptiles.
• Veterinarians and operators of pet stores should advise reptile owners always to wash their hands after handling reptiles and reptile cages.
• To prevent contamination of food-preparation areas (e.g., kitchens) and other selected sites, reptiles should be kept out of these areas -- in particular, kitchen sinks should not be used to bathe reptiles or to wash reptile dishes, cages, or aquariums.
REF: MMWR, 44(17), May 5, 1995. ■
Anticholinergic Poisoning Associated with an Herbal Tea --New York City, 1994
Inadvertent anticholinergic poisoning can result from consumption of foods contaminated with plants that contain belladonna alkaloids. During March 1994, the New York City Department of Health (NYCDOH) investigated seven cases of anticholinergic poisoning in members of three families; three of the seven ill persons required emergency treatment for characteristic manifestations. For all cases, manifestations occurred within 2 hours after drinking tea made from leaves purchased commercially and labeled as Paraguay tea -- an herbal tea derived from the plant llex paraguariensis -- which is native to South America.
On March 20, a 39-year-old man and his 38-year-old wife shared a pot of Paraguay tea. Within minutes after drinking the tea, both developed acute symptoms (including agitation and flushed skin). They were transported by ambulance to a local hospital. In the emergency department, the man was disoriented and agitated. Findings on examination included fever (101.2 F), dilated and nonreactive pupils, and dry skin and oral mucous membranes. Anticholinergic poisoning was diagnosed based on clinical findings, and the New York City Poison Center (NYCPC) was notified. After treatment with two doses of intravenous physostigmine, signs and symptoms completely resolved. Findings on examination of the woman included fever (100.8 F), dilated and nonreactive pupils, and dry skin and oral mucosa. Her symptoms resolved without treatment.
Editorial Note: Paraguay tea is made from the leaves of l paraguariensis, a 20-foot-tall holly tree indigenous to Argentina, Brazil, and Paraguay. Common names for the plant include matÚ, yerba matÚ, and South American holly. The leaves contain caffeine, theophylline, and a nontoxic volatile oil but do not contain belladonna alkaloids.
The dominant clinical features of the cases described in this report (i.e., tachycardia, fever, dilated pupils, and flushed skin) are characteristic of the anticholinergic effects associated with poisoning by belladonna alkaloids. In addition, patients responded to physostigmine, the treatment of choice for anticholinergic poisoning. The most likely explanation for the cases in this report is contamination of the Paraguay tea with leaves from a plant containing belladonna alkaloids. Previous reports of inadvertent anticholinergic poisoning resulting from contamination of foods with plants containing belladonna alkaloids have included consumption of hamburger seasoned with seeds from Angels’ trumpet (Brugmansia X candida) and consumption of contaminated honey, Chinese herbs, or porridge.
REF: MMWR, 44(11), March 24, 1995. ■
Self-Treatment with Herbal and Other Plant-Derived Remedies -- Rural Mississippi, 1993
Herbal and other plant-derived remedies have been estimated by the World Health Organization (WHO) to be the most frequently used therapies worldwide. Therapeutic agents derived from plants include pure chemical entities available as prescription drugs (e.g., digitoxin, morphine, and taxol), standardized extracts, herbal teas, and food plants; plant-derived remedies can contain chemicals with potent pharmacologic and toxicologic properties. Although precise levels of use of these remedies in the United States are unknown, in 1991, herbal products accounted for sales of approximately $1 billion. Previous reports about herbal remedies in the rural South have described the use and biologic activities of locally gathered plant species and details of preparation and dosage, but have not determined the prevalence of use of plant-derived remedies in the study population and the prevalence of use of specific remedies. To assess the prevalence of use of plant-derived remedies (excluding prescription drugs) and the prevalence of use of specific remedies in rural central Mississippi, the University of Mississippi conducted a survey.
Case Reports
Case 1. A 55-year-old man who had completed 11 years of education reported using turpentine during the year preceding the survey to rid himself of "seed ticks." The man purchased turpentine at a local drug store and, based on the advice of a friend, poured approximately 4 oz of turpentine onto a sponge and applied the sponge over all surfaces of his body below the neck. He then bathed in a tub of hot water and had onset of a severe burning sensation. To alleviate the burning, he soaked in a tub of cold water. The man subsequently developed blistering on all body surfaces to which he had applied turpentine. He also reported having used aloe as a topical remedy during the preceding year and reported previous use of briar root, castor, garlic, lemon, and sassafras.
Case 2. A 46-year-old woman who had completed 7 years of education reported using castor oil routinely as a laxative and to treat "colds." She purchased castor oil at a discount department store, kept it readily available in her home, and had used castor oil and acetaminophen to treat a cold in her 18-month-old grandchild. She fed the child 1 teaspoon of castor oil mixed with one half of a baby bottle of orange juice. The symptoms resolved. She also reported using aloe, asafetida, catnip, garlic, lemon, and turpentine as remedies during the preceding year and recalled previous use of briar root, chinaberry, corn shucks, and pine as remedies.
Survey
The survey collected information on demographic, socioeconomic, and health variables; medicinal use and knowledge of 25 specific plants or plant-derived substances*; and diseases or symptoms treated with these plants. The 25 plants were selected based on ethnobotanical research conducted in this geographic area. In addition, respondents were asked about their knowledge or use of any other plant-derived remedies to treat specific diseases or symptoms.
*Aloe vera, asafetida, briar root/blackberry, castor/castor oil, catnip, chinaberry, corn shucks/corn silks, dock/yellow dock, garlic, American ginseng, Jimson weed, lemon, life everlasting/rabbit tobacco/rabbit grass, may apple/bitter apple, milkweed, mistletoe, nutmeg, oak, peach/peach seed/peach pit, pine/pinetop, poke/poke salad, sassafras, sage/horsemint, tobacco, and turpentine.
Of the 251 respondents, 178 (71%) reported using at least one plant-derived remedy during the year preceding the survey.
The most frequently used (i.e., used by at least 10% of respondents) plant-derived remedies during the preceding year were lemon (47%), aloe (27%), castor oil (14%), turpentine (12%), tobacco (12%), and garlic (10%). Other plants used for self-treatment included poke and sassafras.
The most common self-reported reasons for using plant-derived remedies during the preceding year included treatment of diseases or symptoms associated with the respiratory system (43%) the skin (20%), insect bites or parasite infestations (11%), the cardiovascular system (9%), and the gastrointestinal system (6% ).
Editorial Note: In this survey of adults residing in rural areas of Mississippi, nearly three fourths of respondents reported having used plant-derived remedies during the preceding year. These data also indicate that plant-derived remedy use was widely distributed among all age groups and was not limited only to older persons in the population. In comparison, in a previous study of herbal remedy use among a national sample of U.S. residents, only 3% of respondents indicated that they had used such remedies during the preceding year. The substantially higher use reported in the population surveyed in Mississippi may reflect methodological differences in the two studies. Specifically, the definition of plant-derived remedies used in this report was more inclusive than the definition of herbal remedies used in the national survey. In addition, higher use in the population surveyed in Mississippi may be associated with socioeconomic and cultural influences in this population. For example, in rural central Mississippi, only 51% of persons aged >25 years had a high school diploma or higher education compared with 64% for the state. Although utilization rates of the health-care system in the survey area are similar to national rates, self-treatment is an important adjunct to receiving formal care in this area.
Some plant-derived remedies reported in rural central Mississippi (e.g., poke and sassafras) contain pharma-cologically active and potentially toxic compounds. For example, both turpentine and castor oil can produce adverse effects if used inappropriately. Use of externally applied turpentine oil for treatment of parasites has been reported previously. Although turpentine oil is a nontoxic and effective counter-irritant when applied to a small area of the skin, cutaneous application of larger amounts has been associated with vesicular eruptions, urticaria, and vomiting. Castor oil is a stimulant laxative that may cause thorough evacuation of the bowels within 2-6 hours of ingestion; the strong purgative action of castor oil also can cause dehydration and electrolyte imbalance, and long-term use may reduce the absorption of nutrients. Because the stimulant effects of castor oil may cause uterine contraction, some authorities have recommended that it not be used during pregnancy; use also is not recommended in infants and young children.
The survey findings underscore the need for physicians, pharmacists, and other health-care providers to consider the possibility of plant-derived self-treatments among their patients and to actively elicit this information when taking a clinical history. In addition, health-care providers should be aware of potential drug interactions, toxicity, and adverse reactions as well as possible treatment benefits that may be associated with plant-derived therapies.
REF: MMWR, 44(11), March 24, 1995. ■
ETIOLOGY, INCUBATION PERIOD AND CLINICAL SYNDROME FOR COMMON FOODBORNE DISEASES
| Etiology | Clinical Syndrome |
| BACTERIAL | |
| Bacillus cereus | a) incubation period 1-16 hours b) gastrointestinal syndrome |
| Campylobacter | a) incubation period 3 to 5 days b) gastrointestinal syndrome |
| Clostridium botulinum | a) nervous system symptoms; blurred or double vision, difficulty swallowing, paralysis |
| Clostridium perfringens | a) incubation period 8 to 22 hours b) low intestinal syndrome -- majority of cases with diarrhea but little vomiting or fever |
| Escherichia coli | a) incubation period 6 to 36 hours b) gastrointestinal syndrome -- majority of cases with diarrhea |
| Salmonella | a) incubation period 6 to 48 hours b) gastrointestinal syndrome -- majority of cases with fever and diarrhea |
| Shigella | a) incubation period 7 to 66 hours b) gastrointestinal syndrome -- fever, and diarrhea -- containing blood, mucus, and pus |
| Staphylococcus aureus | a) incubation period 1 to 7 hours b) gastrointestinal syndrome -- majority of cases with nausea, diarrhea, and vomiting |
| Vibrio cholerae | a) incubation period 5 hours to 3 days b) gastrointestinal syndrome -- majority of cases with diarrhea and without fever |
| Vibrio paraphaemolyticus | a) incubation period 12 to 24 hours b) gastrointestinal syndrome -- majority of cases with diarrhea |
| CHEMICAL | |
| Heavy metals | |
| Antimony, Cadmium, Copper, Iron, Tin, Zinc, etc. | a) incubation period 3 minutes to 3
hours (rarely longer) b) clinical syndrome compatible with heavy metal poisoning -- usually gastrointestinal syndrome and often metallic taste |
| VIRUSES | |
| Norwalk- like agents | a) incubation period 24 to 72 hours b) gastrointestinal syndrome |
| Rotavirus | a) incubation period 24 to 72 hours b) gastrointestinal syndrome |
| FISH | |
| Icthyosarco- toxin (ciguatoxin) | a) incubation period 30 minutes to 30
hours b) clinical syndrome compatible with ciguatera -- usually initial gastrointestinal symptoms followed by dry mouth, paraesthesias of lips, tongue, throat or extremities; a sensation of looseness and pain in the teeth and a paradoxical temperature sensation are characteristic. |
Iowa Dept of Public Health Bulletin (1994); ISU Comm in Cont Educ, June 1994
REF: Penn State Veterinary News, June 1995. ■
TIDBITS
Foodborne Botulism Oklahoma, 1994
On June 30, 1994, a 47-year-old resident of Oklahoma was admitted to an Arkansas hospital with subacute onset of progressive dizziness, blurred vision, slurred speech, difficulty swallowing, and nausea. Findings on examination included ptosis, extraocular palsies, facial paralysis, palatal weakness, and impaired gag reflex. The patient also had partially healed superficial knee wounds incurred while laying cement. He developed respiratory compromise and required mechanical ventilation. The patient was hospitalized for 49 days, including 42 days on mechanical ventilation before being discharged.
The patient had reported that, during the 24 hours before onset of symptoms, he had eaten home-canned green beans and a stew containing roast beef and potatoes.
The stew had been cooked, covered with a heavy lid, and left on the stove for 3 days before being eaten without reheating. No other persons had eaten the stew.
REF: MMWR, 44(11), March 24, 1995. ■
May the Imbiber Beware
Heavy use of acetaminophen (Tylenol and other brands) may be responsible for as many as 5,000 cases of kidney failure in the United States each year, according to a study published last December in the New England Journal of Medicine.
Researchers suggest that taking just one pill daily for a year doubles the risk of kidney disease. They estimate that eliminating heavy use of the drug could reduce the overall incidence of renal failure by 10%.
Although it has long been known that ingesting large doses (15 grams or more) of acetaminophen can damage the liver, researchers reported last December in the Journal of the American Medical Association that much smaller amounts -- 4 to 10 grams -- may have a similar effect when taken by people who haven’t eaten for a prolonged period of time due to illness. They also found that the risk of liver damage appears to be higher in people who drink alcohol and don't eat before taking the drug.
Manufacturers currently recommend that no more than 4 grams (8 extra-strength tablets) be taken in a 24-hour period.
REF: Harvard Health Letter, 20(6), April 1995. ■
Methyl Bromide -- A Definite Maybe
Is methyl bromide really a danger to the Earth’s ozone layer? EPA said "yes" 2 years ago, but now the agency’s not so sure. Why? Because they now know:
• As much as 80% comes from oceans, plus forest and grass fires, not manmade sources.
• All ozone-diminishing products do not ultimately escape to the atmosphere. Most methyl bromide remains in the soil, or is reabsorbed by the oceans, salt marshes, vegetation, and soil.
• The molecule exists for 1 year, much less than the lifetime of chlorofluorocarbons and other ozone-depleting chemicals. Also, some methyl bromide breaks down into harmless compounds.
EPA reserved the right to change its mind if the chemical does not pose a risk to the ozone layer, so stay tuned.
REF: Kansas Pesticide Newsletter, 18(5), May 15, 1995. ■
National Pesticide Telecommunications Network
The National Pesticide Telecommunications Network (NPTN) has changed its hours of operation. Call toll-free: 6:30 a.m. - 4:30 p.m. (Pacific Time) Monday through Friday: 1-800-858-7378 (General Public), 1-800-858-7377 (Medical Profession/ Government Agencies).
NPTN will soon be available on Internet. The Network provides services to the medical, veterinary and professional communities and general public in areas including:
• Pesticide product information
• Pesticide poisoning recognition and management
• Toxicology and symptomatic reviews
• Health and environmental effects
• Clean-up and disposal procedures
REF: Kansas Pesticide Newsletter, 18(5), May 15, 1995. ■
Inerts May be Cause of Certain Irritations
A newly released study published by the American Chemical Society suggests that people who complain of headaches, drowsiness, and eye, nose, and throat irritations due to exposure of indoor insecticides in particular, may be responding to the volatile organic compounds (VOC's) used as inert ingredients and not to the insecticide’s active ingredient. Indoor pesticides typically contain no more than 3 percent active ingredient, and as much as 99.5 percent water and inert ingredients.
High VOC levels may exist for at least several hours following unventilated spray applications, and for the better part of a day following fogger applications. VOC levels have been found to be highest for foggers and lowest for emulsifiable concentrate sprays. The study determined that many general health complaints that may be attributed to indoor insecticide exposure are also consistent with exposure to the inert ingredient VOC’s. The reason there is much greater potential for acute airborne exposure to VOC’s in insecticides is because they have vapor pressures that are much higher than those of active ingredients.
Copies of this study, entitled "Simulated Air Levels of Volatile Organic Compounds Following Different Methods of Indoor Insecticide Application," are available from the American Chemical Society. Call (202) 872-4450.
REF: Kansas Pesticide Newsletter, 18(5), May 15, 1995. ■
PCBs in Fish and Fetal Toxicity
Because PCBs have been associated with spontaneous fetal death in several mammalian species, Mendola et al. examined the relationship between consumption of PCB-contaminated fish from Lake Ontario and spontaneous fetal death in 1,820 women from the 1990-1991 New York State angler cohort study. Prior pregnancies, smoking, and maternal age were taken into consideration in the analyses. Increases in risk of fetal death were not observed based on lifetime estimates of PCB exposure, years of fish consumed, or kilograms of fish eaten between 1990 and 1991, or over a lifetime. The data suggested that eating fish contaminated with PCBs was not associated with an increased risk of recognized spontaneous fetal death.
REF: Environmental Health Perspectives, 103(5), May 1995. ■
Lyme Disease -- United States, 1994
In 1994, 13,083 cases of Lyme Disease (LD) were reported to the Centers for Disease Control by 44 state health departments, 4826 (58%) more than the 8257 cases reported in 1993. As in previous years, most cases were reported from the northeastern and north-central regions (only 86 cases were reported from California).
The risk for infection among persons residing in or visiting areas where LD is endemic can be reduced through avoidance of known tick habitats; other preventive measures include wearing long pants and long-sleeved shirts, tucking pants into socks, applying tick repellents containing N,N-diethyl-m-toluamide ("DEET") to clothing and/or exposed skin according to manufacturer's instructions, checking thoroughly and regularly for ticks, and promptly removing any attached ticks. Acaracides containing permethrin kill ticks on contact and can provide further protection when applied to clothing, but are not approved for use on skin.
REF: MMWR, 44(24), June 23, 1995. ■
FDA Prohibits Use of Lead Solder in Cans Manufactured for Food
Concluding that available toxicological and exposure data for lead demonstrate that the use of lead solder in the manufacture of cans for food packaging may be "injurious to the public health, particularly that of fetuses, infants and children," the Food and Drug Administration issued a final rule June 27 prohibiting its use.
Effective Dec. 27, the final rule allows existing stocks of lead-soldered canned foods to be offered for sale within one year of the June 27 rule, so long as the lead level in such cans "is not such that the food may be rendered injurious to health." Guidances on the level of lead in food, first announced in April 1993, are 80 micrograms per kilogram (80 ppb) for lead in fruit beverages packed in lead-soldered cans and 250 ppb for all other food packed in lead-soldered cans.
REF: Food Chemical News, 37(19), July 3, 1995. ■
Dietary Aluminum Poses No Significant Public Health Risk: FDA-ers
The risk of neurotoxicity or Alzheimer's disease from dietary aluminum is of "no public health significance," a pair of FDA researchers asserted in a poster presentation at the triennial meeting of the International Congress of Toxicology, July 2-6, in Seattle, WA.
Average dietary aluminum intakes in the U.S. were 7 mg/day for adult women, 8 to 9 mg/day for adult men, and 11.5 mg/day for adolescent boys, the poster said. It noted that these intakes are within the guidelines of the World Health Organization's Joint Expert Committee on Food Additives.
The poster also listed four major sources of dietary aluminum, giving a range of the percentage of the total accounted for by each of these sources. They are: (1) grains and grain products (29% to 49%); (2) dairy products (17% to 36%); (3) desserts (9% to 26%); and (4) beverages (5% to 10%).
Food additives, are the major source of dietary aluminum in the U.S. diet. Aluminum cookware contributes little.
Aluminum intake from medical uses (e.g. antacids) may be 100,000 times higher than that from dietary sources, and even this has rarely caused adverse effects and has never been correlated with neurotoxicity or Alzheimer's disease.
REF: Food Chemical News, 37(20), July 10, 1995. ■
Ethics of Show Animal Drug Use Subject of Two Videos
The video, "A Question of Ethics," arose from the recent scandals involving use of beta-agonists and other illegal substances on show animals at youth livestock competitions. The success of this video led to a newly released follow-up, "A Step Beyond A Question of Ethics," which gives more information on how to ensure ethical show animal drug usage. The videos are available through Texas A&M; for more information, call 409-845-6601.
REF: Food Chemical News, 37(25), August 14, 1995. ■
Lettuce was Source of Montana E. coli Outbreak
The U.S. Centers for Disease Control and Prevention (CDC) has officially named lettuce as the cause of an outbreak of E. coli 0157:H7 in Montana that sickened more than 100 people, apparently the largest outbreak of the pathogen since the Pacific Northwest outbreak two and a half years ago.
On August 5 the CDC officially confirmed lettuce as the main source of the illnesses. How the lettuce came to be contaminated is still under investigation, and a traceback from stores to distributors, trucking companies, packing houses, and growers could take months. Officials have said that one theory is that a herd of cattle near a stream that ran into an irrigation pond could have contaminated the produce.
Leafy red, green, and romaine lettuces were the vehicles, but iceberg lettuce was not implicated. The lettuce was identified after a statistical analysis of infected and non-infected people. Not all of the cases were caused by lettuce, but the majority were.
The outbreak has peaked and the lettuce is probably out of the food supply, but secondary infections are continuing.
REF: Food Chemical News, 37(25), August 14, 1995. ■
FDA's BST Labeling Decision Upheld in U.S. District Court
FDA's decision regarding the labeling of rBST milk products was upheld, both because the plaintiffs did not offer evidence that milk from rBST-treated cows differed in any significant way from other milk, and because the consumers' wish for such labeling was not sufficient cause for it to be required. The court upheld FDA's decision that it did not have to perform an environmental assessment under the National Environmental Policy Act.
REF: Food Chemical News, 37(25), August 14, 1995. ■
VET NOTES
HALF OF ALL FEEDLOT CATTLE GIVEN ANTIBIOTICS ROUTINELY
About half of all feedlot cattle are given antibiotics "as a health or production management tool," according to the results of the Department of Agriculture’s Cattle on Feed Evaluation (COFE).
The COFE study, part of the National Animal Health Monitoring System, looked at 3,214 feedlots in 13 major cattle states. The study was designed to be representative of the nation’s feedlot population. The first part of COFE was released in January; the second part, focusing on health management practices, was published last month.
About a quarter of small (less than 1,000 head) operations and 70% of large operations gave their cattle at least one antibiotic, the study found. About 54% of all feedlot cattle, therefore, are given at least one antibiotic in feed (less than 1% of cattle on feed are given antibiotics in water).
More than half of those surveyed at large operations considered their veterinarian to be an "extremely important" source of animal health information, while about a third thought that nutritionists were extremely important. Other sources of information, such as USDA’s Extension Service, universities, producer magazines, producer organizations, feed and animal health salespeople were not considered to be extremely important to more than 94% of those surveyed.
Nutritionists were considered extremely important sources of animal nutrition information by nearly three-quarters of large operations surveyed, followed by feed salespeople at 12%. Nutritionists also topped veterinarians as extremely important sources of "general production information." About a third of large operations named them as extremely important in this category, followed by veterinarians (23%).
One-Third of Cattle on Antibiotics for at Least 90 Days
For those operations using antibiotics as a health or management tool, about a third of the total cattle were on the drug(s) for more than 90 days, while slightly less than a third were on antibiotics for less than 15 days, with the remainder, 38%, falling in between.
About a quarter of small operations kept their cattle on antibiotics for less than 15 days, 42% gave drug(s) for 15-89 days and 32% gave antibiotics for more than 90 days. For large operations, 42% gave antibiotics for less than 15 days; 18%, for 15-89 days and 42% for 90 or more days. Operations placing antibiotics in water did so for much shorter periods of time, usually less than eight days.
Chlortetracycline was the most commonly used drug given in feed, used by 46% of large operations. This was followed by tylosin (43%), oxytetracycline (30%), chlortetracycline/sulfamethazine (27%), tetracycline (7%), sulfamethazine/sulfamethoxine (5%), neomycin (2%), bacitracin (0.5%) and "other" (1%). The report does not give estimates of drugs in feed for small operations.
About 17% of small operations gave long-lasting (label specifies effect greater than 24 hours) antibiotic injections to their cattle during the feedlot period, while about 14% of large operations did.
About 15% of all feedlot cattle were given a regular (less than 24-hour effectiveness) antibiotic shot during their stay at the feedlot. Small operations gave such shots to about 10% of their cattle, while large operations administered regular antibiotics to 16%.
In addition, about 45% of feedlot cattle were given vitamin injections of some kind. The majority of all injections were intramuscular or subcutaneous, and were most often given in the head/neck area.
About 87% of cattle on feed were given a clostridial vaccination of some kind, and 21% were given more than one clostridial vaccination. Nearly all feedlot cattle were given a nonclostridial vaccination of some kind (most usually for infectious bovine rhinotracheitis).
About 84% of all cattle on feed were thought to be infected with worms, and about 93% of such cattle were given treatment for worms. More than 90% of cattle are also treated for cattle grubs and cattle lice, while 74% are treated for mites, 62% for ticks and 56% for flukes.
A number of methods were used for controlling flies, including environmental sprays (53% of operations), pour-ons/dusting powder/animal sprays (36%) and larval-killing feed additives (7%).
Information on the COFE study, and other food animal studies, is available from the Centers for Epidemiology and Animal Health, 970-490-7800 (Internet: NAHMS INFO@aphis.usda.gov).
REF: Food Chemical News, 37(12), May 15, 1995. ■
HORSE OUTBREAKS MAY SIGNIFY 'BAD' FUMONISIN YEAR AHEAD
Speaking at the national meeting of the American Chemical Society, Margaret Miller, of CVM’s Office of New Animal Drug Evaluation, said that while fumonisins did not appear to be a major problem in the U.S. corn supply in 1993 and 1994, the last few months have seen two outbreaks of equine leukoencephalomalacia (ELEM) associated with fumonisin-contaminated corn.
One outbreak in western Kentucky had killed 19 horses so far, leaving 200 other animals at risk. It was traced to white corn screenings that contained fumonisin at levels of 1-40 ppm. Corn for human consumption in the same area contained much lower fumonisin levels, ranging from 26 to 185 ppb.
The second outbreak killed 18 horses in Virginia and involved fumonisin levels in the range of 2.1 to 21.2 ppm.
ELEM is a horse disease of no relevance to humans except that the unusual susceptibility of horses to fumonisins is an early sign that the current crop of corn may have a higher fumonisin level than was the case in ’93 and ’94.
One of the biggest problems in analyzing the fumonisin content of a shipment of corn is finding a sampling method that accounts for the fact that fumonisin content may vary throughout the load.
Fumonisin Risk from Corn Consumption Low Due to Processing, Varied Diet
Fumonisin-contaminated corn products are not a major health threat in the U.S., despite toxicology results that increasingly brand the chemical as a carcinogen.
Patricia Murphy, a food scientist from Iowa State University, for example, attempted to put the mycotoxin in its proper place by noting that it is simply "one of the background toxins in our diet -- among many hundreds that we consume daily."
William Norred, a pharmacologist with the USDA Agricultural Research Service, Athens, Ga., added that the "take-home message" for farmers and consumers is that a few more years of research are needed before it is clear whether fumonisins are a problem of particular concern in the American food supply. The biggest problem, he added, may be concerns raised by other countries that import U.S. corn.
Paul Howard, a biochemist with FDA’s National Center for Toxicological Research, Jefferson, Ark., noted that fumonisin levels in the U.S. diet are far lower than those that have raised epidemiological concern in portions of China and South Africa. Not only do these areas have fumonisin levels in the range of 75-100 ppm, he said (compared to 0.5-2.0 ppm in the American diet), but the people consume more than 90% of their diet in the form of corn products.
REF: Food Chemical News, 37(10), May 1, 1995. ■
EUROPEAN TESTING FOR CLENBUTEROL RESIDUES USING EYE TISSUES, FLUID
European researchers studying detection of clenbuterol residues in food animals have found eye samples superior to liver samples in detecting the residues.
Speaking at the ACS annual meeting in Anaheim, Calif., Dr. Carlos Van Peteghem culled the research from 120 papers presented last summer in Belgium at the Second International Symposium on Hormones and Veterinary Drug Residue Analysis.
He noted that researchers across Europe are searching for new matrices to detect illegal drug use, adding that numerous researchers across Europe have focused on the eye.
The choroid shows clear indication of clenbuterol accumulation at concentrations which exceed those in liver by forty-fold.
REF: Food Chemical News, 37(10), May 1, 1995. ■
MILK DRUG RESIDUES FOR FY 94 REPORTED
The National Milk Drug Residue Data Base is a voluntary reporting program. Data are reported on the extent of national testing activities, analytical methods used, kind and extent of animal drug residues identified, and amount of contaminated milk (and whether it was disposed of properly for non-human use).
The system is designed to include all milk - Grade A, which represents 90 percent of the milk supply, and manufacturing grade milk representing the other 10 percent.
Two states, New York and Oklahoma, began submitting data in April 1993 to pilot-test the data base. At the end of July 1993, all States were requested to begin reporting their testing data. As of October 31, 1994, all fifty States and Puerto Rico were participating in the data base program.
It is important, however, to recognize that since this was a voluntary reporting program, the samples and tests reported did not represent 100 percent of the milk supply from every state. From October 1, 1993 to September 30, 1994, 4,179,108 samples were analyzed for animal drug residues. Of these samples, 3,693 were positive for a residue. A total of 4,589,085 tests were reported on the samples for 14 different families of drugs or individual drugs. Forty separate testing methods were used to analyze the samples for residues.
A sample is defined as representing a load or lot of milk sampled and analyzed. Data are reported by four sources of samples:
1. Bulk Milk Pickup Tanker -- bulk raw milk from a dairy farm.
2. Pasteurized Fluid Milk and Milk Products -- (after pasteurization) finished product in package form or bulk. Includes milk products such as milk, cream, condensed milk and dry milk products, and condensed and dry whey products.
3. Producer Sample -- raw milk obtained from a dairy farm. Samples are reported by the permitting State, rather than by the analyzing State.
4. Other -- milk from silos, over-the-road tankers, etc.
A positive result, as used in this report and in the table, means that the sample was found to be positive for a drug residue by a test acceptable for taking regulatory action in a certified laboratory by a certified analyst, or the milk was rejected on the basis of an initial test by the milk processors.
Specific tests used, and results for the four sources of samples, along with producer vs. regulatory testing results are included in a report "National Milk Drug Residue Data Base," available from the FDA Veterinarian.
SAMPLE RESULTS OCTOBER 1, 1993 - SEPTEMBER 30, 1994
| Source of Samples | Total Samples | Number Positive | Percent Positive |
| Bulk Milk Pick-up Tanker | 3,213,220 | 2,024 | 0.063 |
| Pasteurized Fluid Milk & Milk Products | 61,775 | 3 | 0.005 |
| Producer Samples | 824,132 | 1,634 | 0.198 |
| Other | 9,981 | 32 | 0.04 |
| Total | 4,179,108 | 3,693 | * |
*A summary of the percent positive cannot be provided because there is no uniformity in terms of sampling in the four categories. For example, the Pasteurized Milk Ordinance (PMO) sets forth specific sampling requirements for beta-lactam testing as follows:
1. Bulk Milk Pickup Tanker Samples - samples
are taken daily on every tanker.
2. Pasteurized Fluid Milk and Milk Products - a minimum of four
samples must be tested for each product at each plant every six
months.
3. Producer Samples - each producer must be tested at least four
times every six months.
4. Other - samples are conducted on a random basis.
........................................................................................................................................
TEST RESULTS
| Family/Drug | Total Tests | Total Positive |
| Aminoglycosides | 391 | 0 |
| Gentamicin | 9,509 | 0 |
| Beta-Lactams | 4,310,118 | 7,256 |
| Ceftiofur | 664 | 0 |
| Cloxacillin | 16 | 14 |
| Chloramphenicol | 1,123 | 1* |
| lvermectin | 16 | 0 |
| Macrolides | 278 | 0 |
| Novobiocin | 116 | 0 |
| Sulfonamides | 143,501 | 59 |
| Sulfadimethoxine | 16,312 | 7 |
| Sulfamethazine | 38,968 | 7 |
| Sulfathiazole | 16,243 | 2 |
| Tetracyclines | 51,373 | 41 |
| Other Drug Groups | 457 | 0 |
| Total | 4,589,085 | 7,387 |
*A chloramphenicol screening test run by a State agency for the NDRMMP was reported as positive. Follow-up confirmation testing at the FDA Denver Laboratory did not confirm the screening test finding by the State.
REF: FDA Veterinarian, July/August 1995. ■
CVM Will Look Closely at Sarafloxacin Use, Says Sundlof
The Center for Veterinary Medicine will look closely at how sarafloxacin, the first approved fluoroquinolone for food animals, is being used, CVM Director Steven Sundlof told Food Chemical News on August 22.
Sundlof said that sarafloxacin, which was approved for the treatment of E. coli in chickens, was the ideal test case for monitoring fluoroquinolone use because the poultry business is controlled by a handful of companies. "Approximately 80% of the chickens in this country are raised by 20 companies," he explained. These companies employ about 38 veterinarians, he said, adding that such a small group of veterinarians would be easy to educate and monitor.
In addition, the product's sponsor, Abbott Laboratories, has agreed to keep "fairly detailed records on use patterns" of sarafloxacin, which it will share with CVM. In addition, the company has agreed to monitor for E. coli drug resistance in chickens, since treatment of E. coli is the only approved use of the product. He also stated that chickens are not considered a primary source of E. coli pathogens in humans. Extra-label use (ELU) of the product will not be allowed, since the product is a feed-use (actually drinking-water use) product. "We will take action if this (ELU) is occurring," Sundlof said.
REF: Food Chemical News, 37(27), August 28, 1995. ■
FDA POSITION ON EXTRA-LABEL USE OF IONOPHORE DRUGS
The Food and Drug Administration has received reports alleging the use of the veterinary ionophore drugs (monensin and lasalocid) in lactating dairy cattle rations. Reports indicate that these drugs are used for various unapproved purposes such as attempting to increase milk production and feed efficiency, reduce the incidence of fatty livers, and prevent ketosis.
FDA has not approved any ionophore product for use in the feed of lactating dairy cattle. The Agency currently does not have adequate data on which to base an approval for the use of ionophore drugs for milk production or other uses in lactating dairy cattle.
Extra-label use refers to the actual or intended use of a new animal drug in an animal in a manner that is not in accordance with the drug’s labeling. This includes, but is not limited to, use in species or for diseases or other conditions not listed in the labeling, and use at dosage levels other than those stated in the labeling.
This policy does not allow extra-label drug use in feeds, and it does not apply to non-veterinarians. Thus, only veterinarians are covered by the extra-label drug use policy, and they are not permitted to use drugs for an extra-label use in feed. Dairy farmers, veterinarians, and consultants should be aware that the use of ionophore drugs in lactating dairy cattle rations is illegal drug use. Also, they should be mindful that such illegal drug use practices reduce consumer confidence in the safety of the food supply.
REF: CVM Update, Food and Drug Administration, August 14, 1995. ■
NEUROTOXIC MYCOTOXINS: A REVIEW OF FUNGAL TOXINS THAT CAUSE NEUROLOGICAL DISEASE IN LARGE ANIMALS
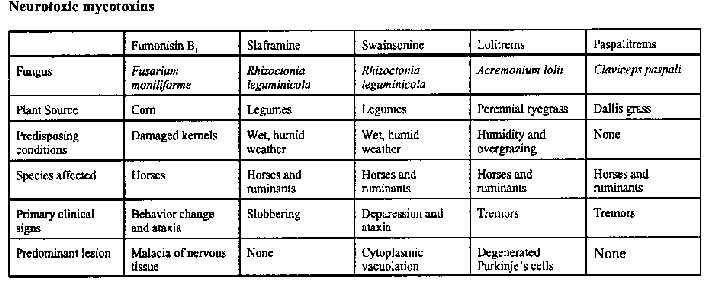
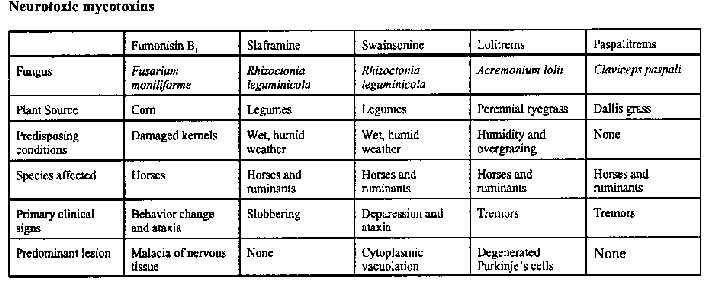
Five mycotoxins found in concentrates or roughages have been shown to cause neurologic disease in livestock. Fumonisin B1 is produced by Fusarium moniliforme and causes leukoencephalomalacia in horses. Swainsonine and slaframine are produced by Rhizoctonia leguminicola and cause mannose accumulation and para-sympathomimetic effects, re-spectively. Lolitrems from Acremonium lolii and paspalitrems from Claviceps paspali are tremorgens found in grasses.
Diagnosis of neurological diseases caused by fungi can be difficult. The clinical signs are often ambiguous or similar to those found in other diseases, and reliable antemortem tests are not available. Histologic lesions may be nonspecific or even absent. Therefore, the diagnosis of diseases caused by neurotoxic mycotoxins depends not only on history, clinical signs, and lesions, but also on finding the specific mycotoxin in the appropriate forage or grain.
Few of the toxigenic fungi that infest feed sources used for livestock produce neurotoxins. Some neurotoxic mycotoxins, such as penitrem A, can experimentally cause disease in livestock; but because they are not produced in common livestock feeds, naturally-occurring disease has not been confirmed. On the other hand, mycotoxins are the suspected etiology for some diseases, such as Bermuda grass staggers, for which the exact etiology is unknown. Yet other mycotoxins can cause neurological signs secondary to hepatic-encephalopathy. This review is limited to the five mycotoxins that cause neurological disease in large animals as their primary effect (see table below).
REF: Penn State Veterinary News, June 1995. ■
Art Craigmill
Extension Toxicologist
UC Davis